Discrimination and dysbiosis: How do social inequalities influence the skin microbiome?

The human microbiome plays an important role in health and disease by helping to regulate key bodily processes, such as our immune response. Maintaining a balanced microbiome is key as imbalances of certain microbes can contribute to various disease states. However, this can be challenging, as multiple factors influence the state of our microbiome and therefore its balance.
Research has so far revealed influence from both genetic and environmental factors, and emerging work has now addressed a potential role for socioeconomic status – which has previously been linked to have a correlation to health status. For example, according to the World Health Organization (WHO), “social factors, including education, employment status, income level, gender and ethnicity have a marked influence on how healthy a person is. In all countries – whether low-, middle- or high-income – there are wide disparities in the health status of different social groups. The lower an individual’s socioeconomic position, the higher their risk of poor health” [1].
Here, I explore the role of socioeconomics and other potentially discriminatory factors in influencing human health via the microbiome, with particular focus on the findings of a recent review paper [2].
The microbiome and its role in health and disease
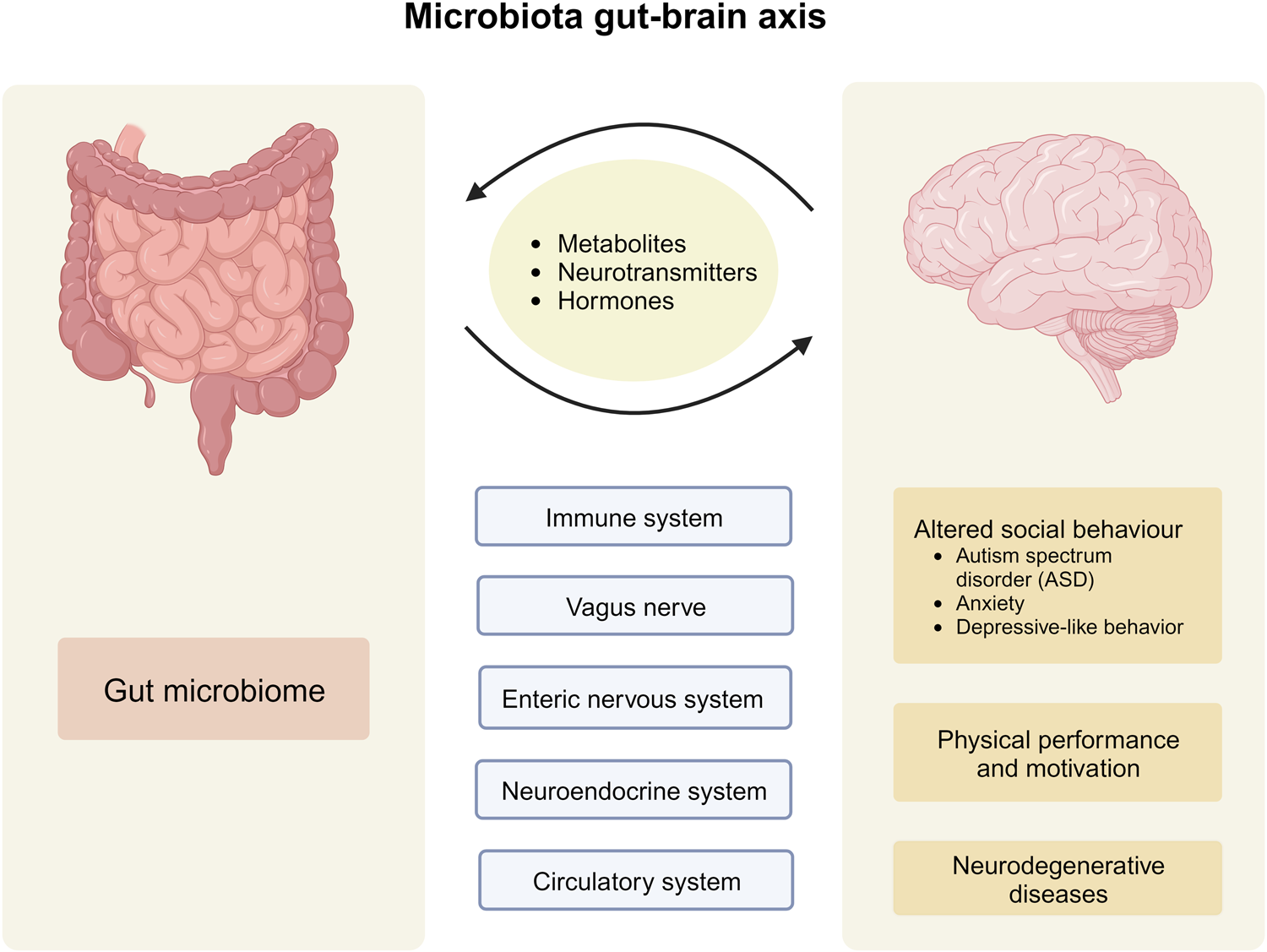
Research over the last 2−3 decades has unravelled numerous implications of the human microbiome for human health and disease [3]. As the vast majority of the microbiome is located in the intestinal tract, most of this research has logically focused on the intestinal microbiota [4]. Although real cause−effect relationships are still scarce, it has turned out that the structure (species inventory) and function (physiological activities) of the human microbiome show significant associations, not only with intestinal disorders but also more distant diseases, including, for instance, liver, heart, lung, skin, metabolic and neurological diseases. From the intestinal tract, microbes can physiologically reach out across the whole body using metabolic, immunological or neurological pathways.
The skin microbiome itself has also been shown to be a core component of health – primarily as it can influence the function of our protective skin barrier and our immune responses. Skin-resident microbes, for example, help maintain a stable skin environment and can regulate our inflammatory response or trigger an immune reaction when threatened. However, if disrupted, variations in our normal skin microbiome composition can lead to inflammation and challenge our immune systems [5,6].
Understanding the microbiome and its role in health and disease has been a key area of research in recent years. Although there are still many paths to be explored, this work has unveiled numerous factors that can contribute the balance – or imbalance – of the human microbiome.
Exploring factors influencing the microbiome
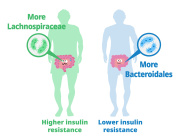
Microbiome research is highly challenging, especially when shifting from strictly controlled animal models to humans in real life, as many factors affect the structure and function of the human microbiome. These factors include endogenous (genetic) and exogenous (environmental) ones. For example, your age, gender, race and certain hereditary elements have been found to help determine your microbiome structure, as well as external conditions such as climate and living environment [7,8,9,10].
Now, recent research has suggested that your socioeconomic status should also be counted among the latter. An excellent review on ‘The human gut microbiome and health inequities’ [2] proposes that discrimination-related experiences are likely to affect the structure and function of the microbiome through numerous pathways. The authors suggest that discrimination due to socioeconomic status, as well as race, gender and sexual identity, can negatively affect several environmental factors known to be important for the development and maintenance of a healthy microbiome, such as:
- Dietary quality, quantity and diversity e.g. lack of dietary fibres
- Breastfeeding duration
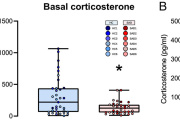
- Stress and abuse e.g. alcohol, cigarettes or other drugs
- Access to safe outdoor spaces, allowing contact with a diverse and healthy outdoor microbiota
- Pollutant and pathogen exposure e.g. due to air and/or drinking water pollution
- Circadian dysregulation e.g. due to shift work
Such factors might negatively affect the human intestinal microbiome and lead to acute and/or chronic disease symptoms and/or a weakened immune system. The medications or therapies (e.g. antibiotics) required can result in further and long-lasting microbiome perturbations.
Studies linking microbiome and health inequities are still scare. Nevertheless, the authors assume that the structure and function of the microbiome of minoritized populations (i.e. groups that are mistreated or discriminated against) not only reflects patterns of structural inequities, but might also be conserved and even amplified over future generations, as the microbiome is passed from mothers to children. Consequently, the microbiome also appears as a novel target to fight against discrimination-based health inequities.
Health inequalities and the skin microbiome
In the review, the authors present convincing evidence linking health inequities and the gut microbiota. Although the studies addressed by the review do not explicitly address health inequities and the skin microbiome, it is well known that social disparities also exist for skin diseases [11]. In addition, in view of the fact that the human gut and skin microbiota and gut health and skin health are linked via the gut–skin axis [12], it is reasonable to assume that the effects of health inequities for the gut microbiota are also relevant for skin health.
Here I will briefly highlight one line of discussion from the review that also holds relevance for the skin microbiota (but see ref. 2 for more details on the underlying original studies). Vaginal birth, breastfeeding and regular skin-to-skin contact represent good opportunities for an exchange of beneficial bacteria between mothers and their children. However, caesarean births are more frequent in low socioeconomic and minoritized populations and go along with increased exposure to antibiotics. In addition, mothers with low socioeconomic status, or in minoritized populations, shift from breast to formula feeding earlier and engage less in skin-to-skin contact than those in higher socioeconomic or more general populations; for instance, due to higher maternal work pressure and/or a lack of health knowledge. Formula-fed children not only miss the pro- and prebiotic ingredients of breastmilk, but are also more likely to come into contact with water-borne pathogens and toxins.
Workplace efforts that allow mothers to produce breast milk throughout the day appear to be a good starting point to counteract such trends. However, they do not account for potential negative effects of freeze–thaw heat cycles on breast milk composition, and they reduce mother–infant physical contact. Consequently, longer periods of paid maternal leave would be a better option, also from a microbiome and child health perspective.
Avenues for future research
The above is just one example of how microbiome-based knowledge might help to initiate and substantiate political and practical measures to ameliorate health inequities.
The authors stress that more research is needed to better understand the microbiology of minoritized and discriminated populations, and the weight of the influence of the different contributory factors [11]. They also criticize that most (gut) microbiome studies target relatively homogenous populations of adults of European descent living in high-income settings, and so research exploring a more diverse study population is important. Additional research to build a better picture of how the skin microbiome specifically is affected is also key to understanding how the different factors that influence the microbiome relate to and work with or against one another.
Progress in this field clearly requires closer collaboration between microbiome scientists, epidemiologists and social scientists to better elucidate and address the relationship between socioeconomics, the human microbiome (both gut and skin) and health and disease.
Read more in the blog of Dr. Markus Egert, active member of ISM scientific committtee
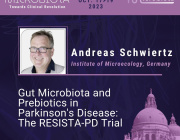
Targeting Microbiota 2023 this October will dedicate a session to social inequalities and the microbiome. Submit a related abstract.
Media contact:
International Society of Microbiota
[email protected]
Targeting Microbiota 2023 Congress
October 18-19, 2023
Website | LinkedIn | Facebook